
From Jill Brown Photography
Dear Melissa,
One of my “regulars” was recently diagnosed with diabetes. She's on medicine for it. Does this impact how she is able to participate in my indoor cycling classes? What do I need to know?
Sincerely,
G.H., Concord, NH
In response to G.H.'s excellent question, here is a crash course on diabetes treatment and how to maximize your riders' safety.
Shortest Background Section Ever
I could write ten pages on diabetes -- but you'll probably stop reading before you get to The Good Stuff. So let us begin with the barest-bones background required for working with clients who have diabetes.
There are two basic “kinds” of diabetes.
Type 1 (DM-1) is an autoimmune disorder with typical peak onset in childhood-young adulthood (but can occur at any age) characterized by antibodies against pancreatic beta cells, the cells responsible for producing insulin. Insulin is one of the “mastermind” hormones, responsible for governing how the body uses fuel. Without insulin, the body cannot absorb glucose out of the blood stream and into working tissues that it needs for fuel.
Type 2 diabetes (DM-2), in contrast, is a state of insulin resistance. Typically associated with obesity and its resulting metabolic/hormonal disturbances, patients with Type 2 diabetes do make insulin early in the disease — but tissues stop being sensitive to it, and thus cannot use it for fuel. In response, pancreatic beta cells release even more insulin — and more insulin, and more insulin — but the tissues still cannot use it. Eventually, the beta cells “burn out” and the disease is characterized as both insulin resistance AND insulin depletion. Recent projections predict that by 2050, 1 in 3 American adults will have DM-2.
The Stakes are High
Complications of uncontrolled diabetes are vast. There are microvascular (small vessel) complications, caused by these vessels becoming chronically coated with toxic amounts of glucose and metabolites: kidney disease that can eventually require dialysis, damage to the retina that can lead to blindness, and damage to the body's longest nerves in the feet, legs, and hands that leads to problems ranging from numbness/loss of sensation, to a burning-type pain that is very difficult to treat, to ulcers and infections possibly resulting need for amputation. There are also macrovascular (large vessel) complications in the heart and brain: Patients with diabetes are at least twice as likely to incur a heart attack or stroke (and more likely to die from either).
Treatment of Diabetes Mellitus
Again, let's keep this simple. We have two principles of diabetes treatment:
Avoid the complications of chronically elevated blood glucose, a described above;
Avoid hypoglycemia (blood sugar that is too low, typically thought of as < 70), which has its own dangers if untreated. Hypoglycemia usually resolves quickly (by eating/drinking glucose) — but if left untreated, it can lead to confusion, fainting, or more seriously seizures or even death. Avoiding this is key.
With these principles in mind, diabetes treatment can be broken down into oral medications and injected medications, the latter most commonly to include insulin. We make treatment decisions based on the pathophysiology of the disease. In DM-1, folks do not make enough insulin — thus, their treatment is always to be given insulin. In DM-2 wherein folks either make insulin (but are resistant to insulin) or do not make insulin (such as in the case of “beta cell burnout”), treatment varies accordingly.
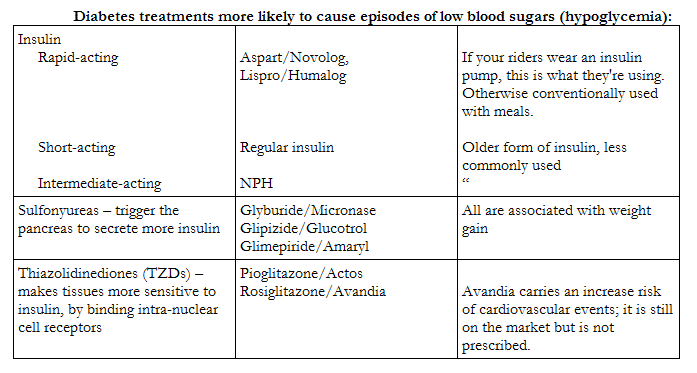
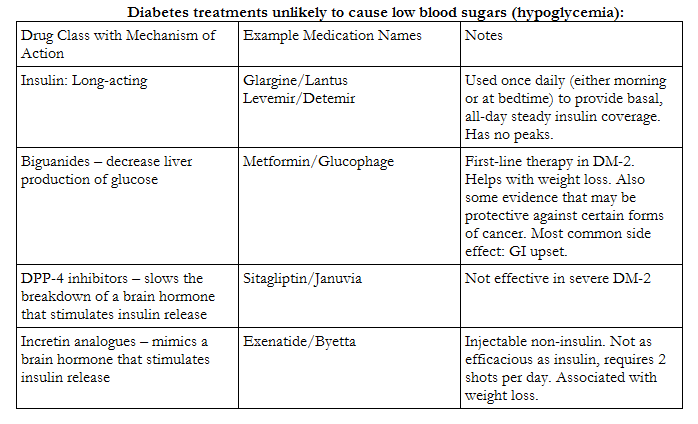
There are many different types of DM-2 treatment that target various points in the body's glucose processing and insulin-responding pathways. Some reduce the liver's production of glucose; some make body tissues more sensitive to insulin; some make the pancreas secrete more insulin; some mimic the hormones in the brain that control insulin release. Each class of medications carries with it certain benefits (i.e, greater efficacy, weight loss) and side effects (i.e., weight gain, cardiovascular risks, hypoglycemia). Patients with DM-1 need to be on insulin since their pancreas is not releasing their own. In DM-2, there is some evidence that using more aggressive therapy (i.e., insulin) early in milder disease vs. waiting until the disease progresses can minimize severe disease complications; more commonly, however, the treatment algorithm for DM-2 proceeds in an orderly progression from metformin to other oral agents to insulin. Treatment decisions should be a collaborative process between patients and their clinicians, to account for this balance between risks and benefits in the context of the patient's other medical conditions, lifestyle considerations, goals and values.
I am happy to explain all of these medications in a later piece. For now, here's what you need to know about the most commonly used diabetes medications that your riders may tell you they're taking:
Finally, What You Asked For: How Diabetes Impacts Exercise
Exercise is an important part of the non-pharmacologic treatment for diabetes mellitus, by reducing cardiovascular risk in both DM 1 and 2 and by improving glycemic control in DM-2 (through weight loss and improved insulin sensitivity). The American Heart Association and American Diabetes Association recommend at least 150 minutes of moderate-intensity or 90 minutes of vigorous aerobic exercise per week. Note use of the word “aerobic.” Everyone with a major medical condition affecting the cardiovascular system should consult with their physician regarding the intensity of recommended exercise — given the severity of cardiovascular complications and individual conditioning levels, some patients may be advised to avoid high intensity anaerobic exercise. Other restrictions may apply, depending on the level of complications. Folks with proliferative retinopathy should avoid anything that causes a dramatic increase in blood pressure (i.e., heavy weight lifting) because this may cause bleeding within the eye. Those with severe neuropathy in the feet should take care to avoid intense high-impact activity (i.e., running, Step aerobics) and be careful to wear well-fitting protective footwear to minimize the risk of ulcerations.
And now to talk about what happens to blood sugar. In folks without diabetes, the body has a functioning regulatory mechanism to control insulin release and blood sugar during exercise. For many of your clients with diabetes, these regulatory mechanisms do not work properly — nor do they apply to exogenously injected insulin. During exercise, increased temperature and blood flow may increase insulin absorption — which drops blood sugar. For DM-2 patients on oral drugs, blood sugar may also drop during exercise depending on timing with meals.
As described previously, we need to take care to avoid hypoglycemia in patients with diabetes. If your riders state that they “feel funny,” you should be aware that this may be what is going on. Many people describe feeling light-headed, woozy, dizzy, nauseated, clumsy, shaky, twitchy, or sweating profusely.
The most common cause of exercise-induced hypoglycemia is inadequate replacement of carbohydrates before, during, and after exercise. This is further complicated if your student is also taking a beta blocker. Folks most commonly become aware that they “feel funny” (sweating, fast heart rate, and other symptoms caused by activation of the sympathetic nervous system). You may recall from my previous article (https://www.indoorcycleinstructor.com/icipro-instructor-training/icipro-team-member-articles/melissa-marotta/beta-blockers-qa/) that beta blockers inhibit many of these sympathetic nervous system signals — thus, many people experience “hypoglycemic unawareness.” This means what it sounds like: folks are unaware that their blood sugars are low, and thus do not take actions to address this. This is very dangerous.
Suggested modifications that your clients can do to enhance their own safety:
More frequent fingerstick blood glucose monitoring (at least to start, to gather data about how their body responds to different forms/conditions of exercise) — before, during and after exercise. They should pay attention to the effects of time of day, timing and content of meals. For those using insulin injections, they should also pay attention to the timing of injections (generally 60-90 minutes before exercise), and effects of various injection sites (arm vs. leg vs. abdomen), remembering that insulin is absorbed faster from an exercising muscle.
Work with their physician/certified diabetes educator to develop a plan for insuling reductions — particularly for those on a continuous insulin infusion pump. Generally insulin requirements are reduced by 30% during exercise.
For those on any of the oral medications in my “Likely to Cause Hypoglycemia” chart above, they should document their low blood sugars and review them with their physician/CDE.
Since the risk of hypoglycemia extends until 4-8 hours after exercise due to glycogen depletion, folks should consume a slowly absorbed carbohydrate (i.e., whole grains) immediately after exercise
Always come to class/the gym with a source of 15-30 grams of quick glucose: juice, a glucose gel or tablet
This is a lot of information, I know. So let us finish off with a recap.
What You Can Do — Right Now — to Improve the Safety of Your Clients with Diabetes:
1. Ask what medications they”™re taking (refer to my charts to see if their meds are likely/unlikely to cause lows). If they”™re not on anything in the former category, you can generally stop here.
2. Ask if they check their blood sugars. Ask them if they get hypoglycemic episodes/”lows,” and if they can tell when they happen.
3. Ask if they have any restrictions from their physicians as to exercise intensity. Encourage them to discuss exactly what happens in an indoor cycling class with their physicians, as most have no idea.
4. Remind them to always have an emergency glucose supply with them (quick carbs) and to bring a whole grain snack to consume immediately thereafter.
As coaches and instructors, we should encourage the folks we train to refuse to be defined by their chronic medical conditions. With proper planning and attention to safety, we can ensure that our riders derive a meaningful and a rewarding experience from our indoor cycling classes. By educating yourself about these important safety concerns, you are one step closer to being an important resource for those who need you.
The author is in her final year of medical school at the University of Vermont College of Medicine, in Burlington, Vermont. She is also a STAR 3 Spinning(R) instructor, ACE-Certified Personal Trainer, and author of the popular coaching motivation blog, Spintastic (http://spintastic.blogspot.com/). Her research interests include health literacy, patient-physician relationships, and the psychological effects of Heart Rate Training.
Do you have a question that you would like addressed by the ICI Medical Research Correspondent? E-mail melissa.marotta@uvm.edu.
References:
Chipkin SR, Klugh SA, Chasan-Taber L. (2001). Exercise and diabetes. Cardiol Clin. Aug;19(3):489-505.
Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, Chasan-Taber L, Albright AL, Braun B (2010). Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association joint position statement. Diabetes Care Dec;33(12):e147-67.
McKulloch DK (2011). Effects of exercise in diabetes mellitus in adults. UpToDate.http:// www.utdol.com/
National Diabetes Information Clearinghouse (NDIC) Information Sheet. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute of Health. http://diabetes.niddk.nih.gov/dm/pubs/stroke/#risk
Center for Disease Control (CDC). Number of Americans with Diabetes Projected to Double or Triple by 2050. 22 October 2010. www.cdc.gov
Note: Melissa is getting close to being called Dr. Melissa. The crush of work necessary to complete her degree has left her with little time for anything else, hopefully explaining her infrequent postings. We certainly appreciate hearing from you when we can Melissa! John

Thank you, soon-to-be-Dr. Melissa. Your medical knowledge and insight are invaluable. I especially like the line about not being defined by medical conditions. The same goes for age. Bravo.
Thank you so much for your kind post, Marsha! (Sorry for my delinquency in catching up with comments!). I very much appreciate that you took the time to say that you got something out of my blabbering 😉